back to all blog posts
Central City Concern is Preferred Partner for MOUD Pilot Program
Monday, February 5, 2024A new pilot program, kicking off in February, will save hundreds, maybe thousands of lives.
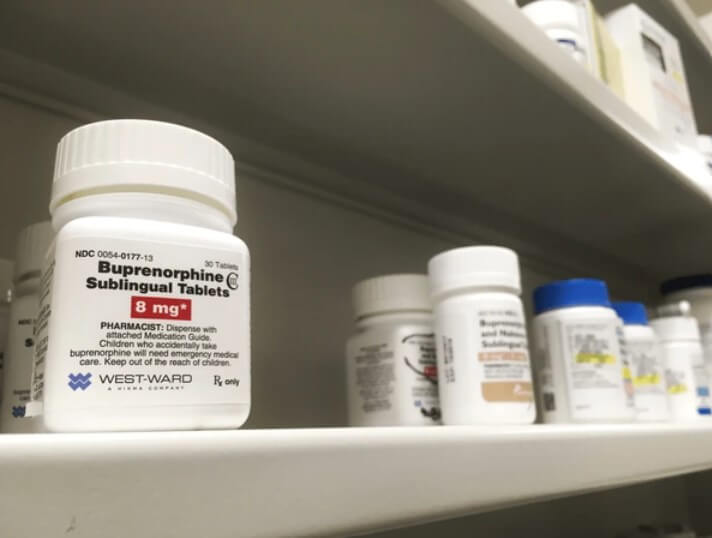
Central City Concern (CCC) has been identified as the preferred partner in Portland Fire & Rescue’s new Mobile Medication for Opioid Use Disorder (MOUD) pilot program, which will begin treating people for opioid addiction immediately (or shortly) after they are revived from an overdose. This involves offering immediate access to buprenorphine and connections to longer-term treatment and recovery services. Members of Portland Fire and Rescue’s Community Health Assess and Treat (CHAT) team will administer these life saving medications as well as make referrals to CCC’s Blackburn Center and Old Town Clinic.
“CCC is a tried and true expert,” says Multnomah County Health Officer Richard Bruno, who recently served as CCC’s senior director of health services. “Providers [at CCC] are known throughout the region for providing excellent cutting edge substance use treatment for people.”
Modeled after successful programs in Maryland and California, the program will provide low barrier access to buprenorphine, a medication for opioid use disorder, to combat the symptoms of opioid withdrawal. “This gives us a new tool to be able to help people not only get started on medication, but to plug them directly into treatment and care that we haven’t necessarily been able to mobilize in the past” says Dr. Bruno.
After a patient is revived from an overdose, consenting patients will receive the medication and a referral to one of CCC’s clinics once their condition has stabilized. The patient will then meet with a clinician for a same-day appointment, including a medical evaluation and a prescription for buprenorphine. The goal is to establish ongoing care with the patient and connect them to CCC’s continuum of wraparound support such as recovery and housing services.
Coming Together in a Community of Care
“I was super honored they identified us as their preferred partner,” says Dr. Amanda Risser CCC’s senior medical director of substance use disorders who consulted heavily on the plans for this program. “It’s always been a vision of ours to be a low barrier, compassionate center of excellence for providing folks with buprenorphine.” Risser collaborated with a team of key stakeholders including healthcare and emergency services who lent their collective expertise to develop this program.
What is Buprenorphine?
Buprenorphine is classified as a partial opioid antagonist and helps break the cycle of the intense and uncomfortable symptoms of opioid withdrawal.
“If you’re able to offer somebody buprenorphine in the short period of time after they receive Narcan (brand name for the nasal spray naloxone), their discomfort will be improved,” says Dr. Risser. When someone is revived with naloxone after an opioid overdose, they emerge in immediate withdrawal, causing extreme discomfort with symptoms such as nausea, vomiting, rapid heart rate, and sweating. Because of buprenorphine’s ability to mimic some of the effects of an opioid, it mitigates some of the more uncomfortable effects of withdrawal. Being able to combat the cycle of withdrawal and give the patient some comfort gives them the physical and mental capacity to be able to navigate their options for medication and recovery services.
Lives Can be Saved
Research shows medication such as buprenorphine save lives, but barriers to access have historically kept this medication out of the hands of those who need it most. “Only 10-15% of folks who really could utilize this medication are taking it” says Dr. Risser, “There’s so many barriers that they may feel like it’s not a viable option for them.” Barriers, such as access to the drug in emergency rooms and stability criteria, have historically made it hard for people to get a prescription. By lowering these barriers, lives can be saved. “Study after study shows us as a medical community that providing folks with low-barrier access to this medication is the right thing to do” says Dr. Risser, “This medication is life saving in almost every context.”
Breaking the Cycle For Good
“We hear from our firefighting colleagues they often respond to multiple calls for the same person” says Dr. Bruno, “Time after time, we have people stuck in a pattern of use, (overdose) reversal, use and reversal.”
The incredibly addictive nature of opioids can sometimes keep people from getting into recovery, even if they want to, because of how horrible drug withdrawal feels. Research shows the next dose after an overdose is especially dangerous: “We know from emergency department research that people who have been revived from an overdose have a 5% risk of death in the next year” says Dr. Risser, “And that risk is highest in the first 48 hours after their overdose.”
Because of the withdrawal mitigating effects of buprenorphine, extending comfort to a person who would otherwise be in the throes of withdrawal allows a person the physical and mental capacity to navigate their options for medication and recovery services. It also keeps them from using that next, and potentially fatal dose. As Dr. Risser puts it: “If we can provide somebody with medication to reduce that risk, and pretty much immediately after starting buprenorphine, somebody’s risk of death is cut in half, then you can hopefully keep that person alive and on medication that helps them reduce or stop their use. This reduces the risk of overdose death in the future.”
Extending humanity is why dedicated clinicians like Dr. Risser work to make these medications accessible, so patients know their survival matters. As Dr. Risser puts it, “I’m hoping by participating in this pilot with CHAT, and in the everyday work we do to treat folks with substance use disorders, people get the message,’you matter to us. We care about what happens to you, we want you to be comfortable, we want you to be safe, and we want you to survive.”
“I’m hoping by participating in this pilot with CHAT, people get the message, ’you matter to us. We care about what happens to you.” – Dr. Amanda Risser